Anterior Cervical Discectomy and Fusion
Told you need neck surgery? Let me explain what the patient can expect from an anterior cervical discectomy and fusion, commonly referred to as ACDF.
We’ll begin with breaking down the name: anterior cervical discectomy and fusion. Anterior refers to the direction in which the surgeon approaches the patient’s body, and cervical refers to the location where the surgery is conducted.
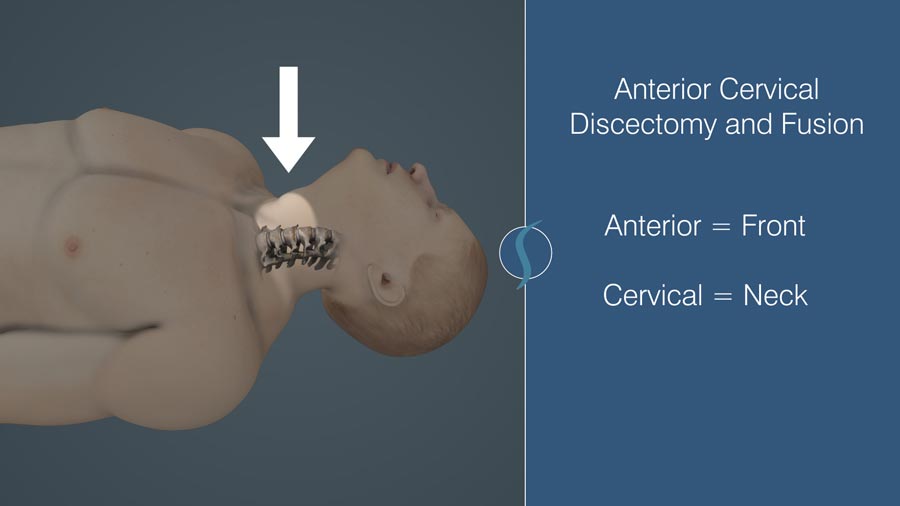
In other words, the surgeon makes an incision in the front (anterior) neck (cervical). The incision is not only skin deep. Care is taken to safely dissect between various muscle groups and avoid damage to other important structures. The esophagus, trachea, and major arteries and veins are carefully retracted, allowing the surgeon to visualize the targeted spine area..
Discectomy refers to the removal of the herniated disc material. Once the surgeon has reached the bones of the neck and located the targeted disc, the disc material is removed. Without the pressure from the herniated disc, the surrounding tissues — such as the thecal sac, spinal nerves, and spinal cord — are no longer irritated. Any compressing bone spurs are also removed at this stage.
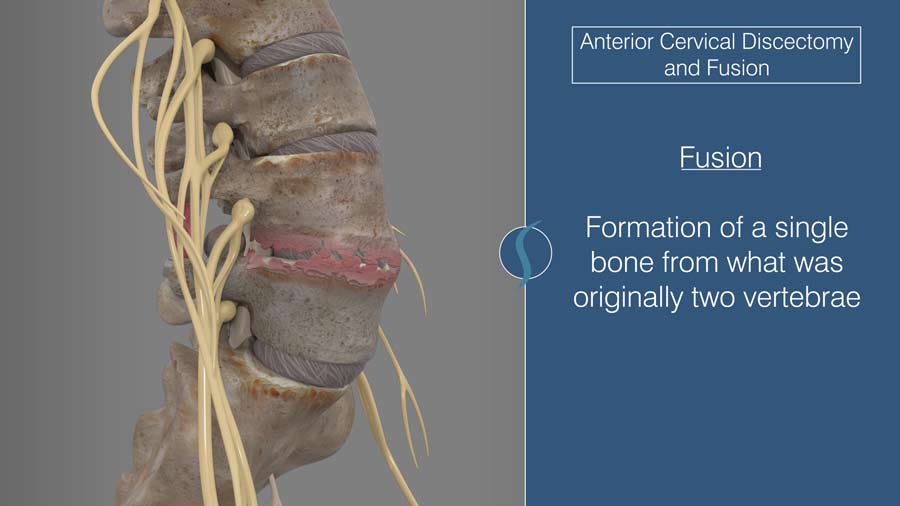
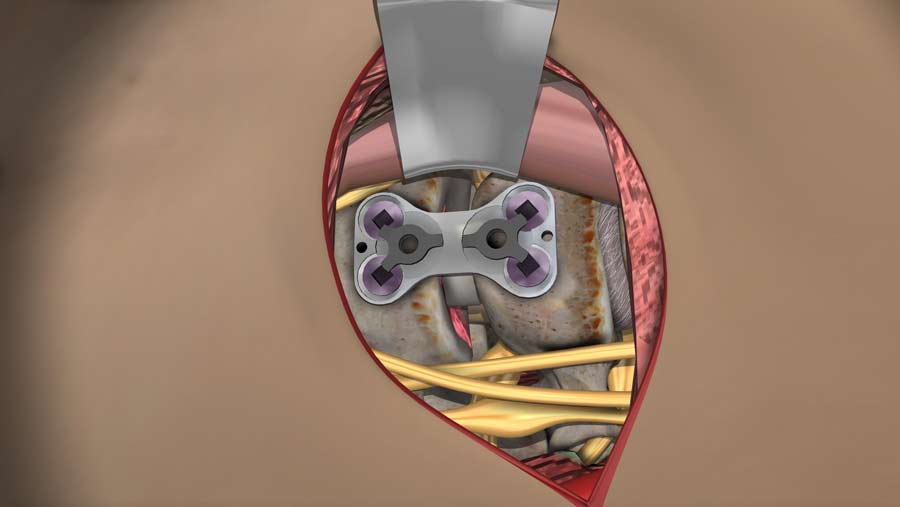
Now, fusion, as the name implies, refers to the formation of a single bone from what was originally two vertebrae. The bone edges are scraped clear of soft tissue and contoured appropriately to accept the bone graft or cage that is placed into the empty space that contained the removed disc. The bone or cage then heals together to complete the fusion process. Care is taken to select the appropriately sized graft or cage to fit into the disc space. Usually , a combination of plates and screws provide stability while the bone grows into the graft.
Upon graft completion the surgeon returns all the structures to their proper place and the incision is closed. A cervical collar may be recommended depending on the patient and the intensity of the procedure. As expected, certain activities may be restricted while your body recovers from the operation. Specific questions and individual concerns should be discussed with your surgeon.
Why Get It?
ACDF is the preferred surgical intervention for symptomatic cervical spine herniations or bone spurs that compress the spinal cord or nerve roots. The most well-studied and well-established causes for ACDF are radiculopathy, and myelopathy.
Those with radiculopathy caused from a pinched nerve are often able to improve with non-surgical treatment. One study shows that most patients showed improvement in their symptoms within 4 to 6 months. As emphasized in my prior videos, ACDF should only be considered when all non-surgical or conservative treatments have been exhausted.
Concerns
The presence of spinal cord compression symptoms, or myelopathy, can be a significant reason for pursuing surgery. Upon the surgeon’s confirmation of the diagnosis by clinical findings, a surgical intervention should be considered. Severe symptoms of myelopathy are more than numbness and radiating pain in a dermatomal distribution. If there are severe weakness of the legs, or inability to control your bladder and bowels, you must be evaluated immediately. .
Supporting Research
Studies have shown the efficacy of an alternative surgery, cervical disc arthroplasty or disc replacement. It may preserve cervical motion and potentially reduces the risk of adjacent segment degeneration compared to ACDF.
Additionally, other non-fusion alternatives are available and preferred in some scenarios. Currently, research is being aimed at improving fusion with 3D printing. The goal being to improve patient outcomes.
For a long time, ACDF has and still remains the standard surgical intervention for managing symptomatic disc herniations. Despite boasting a relatively high success rate and low complication rate, it does have room to improve. New technological advancements may result in even better surgical techniques and better patient outcomes.
I hope this video broadened your understanding of ACDF. Until next time, this is Dr. John Shim.
Additional References:
https://thejns.org/spine/view/journals/j-neurosurg-spine/10/4/article-p343.xml
Citations
- Bydon M, Mathios D, Macki M, de la Garza-Ramos R, Sciubba DM, Witham TF, Wolinsky JP, Gokaslan ZL, Bydon A. Long-term patient outcomes after posterior cervical foraminotomy: an analysis of 151 cases. J Neurosurg Spine. 2014 Nov;21(5):727-31. PubMed PMID: 25127430
- Clarke MJ, Ecker RD, Krauss WE, McClelland RL, Dekutoski MB. Same-segment and adjacent-segment disease following posterior cervical foraminotomy. J Neurosurg Spine. 2007 Jan;6(1):5-9. PubMed PMID: 17233284
- Platt A, Gerard CS, O'Toole JE. Comparison of outcomes following minimally invasive and open posterior cervical foraminotomy: description of minimally invasive technique and review of literature. J Spine Surg. 2020 Mar;6(1):243-251. PubMed PMID: 32309662
- Leveque JC, Marong-Ceesay B, Cooper T, Howe CR. Diagnosis and Treatment of Cervical Radiculopathy and Myelopathy. Phys Med Rehabil Clin N Am. 2015 Aug;26(3):491-511. PubMed PMID: 26231961
- Woods BI, Hilibrand AS. Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment. J Spinal Disord Tech. 2015 Jun;28(5):E251-9. PubMed PMID: 25985461
Last modified: February 24, 2021









