Anomalies That Can Affect Your Back Surgery
In the last video, we concentrated on test findings in your neck that could influence your surgical treatment options. In this video, I will be sharing the test findings in your lower back that could affect your options.
One of the most common variants is the presence of a missing or extra lumbar bone. This condition is called Lumbosacral transitional vertebrae.
In the former scenario, we refer to it as sacralization of the lumbar vertebrae. The last open disc level is the L4-S1 level instead of the more common L5-S1 level. In other words, there are only 4 lumbar vertebrae.
At times, a viewing of X-rays, MRIs, and CTs of the spine is needed to identify the proper level of the anomaly. Certain studies will allow identification of the variant.
Without all the studies, Physicians can number the locations of certain discs differently, and potentially cause an issue during intervention.
In the other scenario, it’s lumbarization of the Sacrum. There are 6 lumbar vertebrae instead of the standard 5, which can again lead to a potential misinterpretation of the Studies.

Around 8-10% of the population exhibits either an extra or missing lumbar vertebrae.

In order to prevent any discrepancies between different readers, the interventionist should consider this anomaly in their interpretation and planned procedure.
Our next variant is the Spina Bifida Occulta.
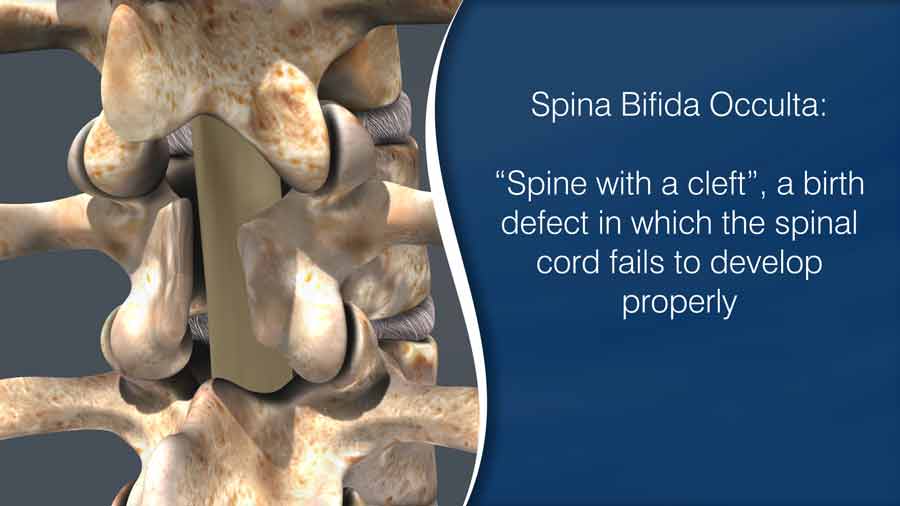
Spina bifida in Latin means “ spine with a cleft” or “spine divide”. At its most extreme, the spinal canal is open along several vertebrae exposing tissues and nerves.
In its more subtle form, the baby is born with a minor cleft in the spine. This small gap does not cause any disabilities and is considered incidental without consequence — and can occur in up to 10% of the population.
For patients about to undergo surgery, this missing bone covering over the nerve tissues may become an issue if the surgeon hasn’t identified it in your test results.
With the use of mechanical instruments and high speed drills, not anticipating this cleft can put the softer tissues at risk for injury.
Our last variant is the Conjoined nerve. For this condition, the nerve pathway from the spinal cord differs from the standard exit out of the neuroforamen.
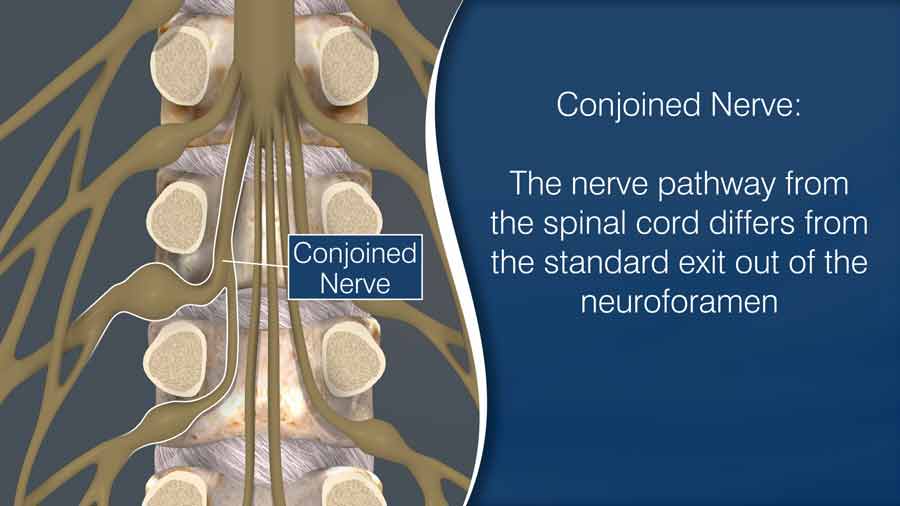
Most people would never know they have such a path, but if you have this variant and you schedule a spine surgery, the location and direction of the nerve need to be considered in the surgical approach. In a prior video, I discussed where and how the surgeon decides to make the incision.
Sometimes, the incision and surgical approach need to be adjusted to accommodate the conjoined nerve. Sometimes, the conjoined nerve requires additional removal of bone and spine stabilizers. This accommodation may require a more invasive fusion technique to safely achieve the operation’s goal.
The conjoined nerve may not always be apparent on standard diagnostic testing. When needed, I have ordered dye based tests, such as a myelogram followed with a CT scan, to better understand the patient’s conjoined nerve pattern. I typically would not order such an invasive test unless a surgery was planned.
If the MRI result includes the possibility of a conjoined Nerve root, the surgeon must consider various dissection pathways to achieve the surgical goal. Also, the patient with a conjoined nerve could be alerted that they might have higher rates of nerve irritation after the operation.
Reports of transitional vertebrae, spina bifida occulta and conjoined nerve roots may cause the surgeon to consider alternative surgical approaches. If you see these or any other findings on your diagnostic testing reports, your surgeon may have already considered these findings. At the same time, most surgeons do not mind discussing these findings with you. You, as a well-informed patient, will understand the risks as well as the benefits of surgery and be better prepared for the outcome of the operation.
Thanks for reading.
Referenced Video: Where to Make the Incision?
Last modified: November 12, 2020









