Why am I Still in Pain After Spine Surgery?
PART ONE
How come I’m still in pain after spine surgery? It’s a common question, and the answer depends on the type of surgery and when you ask.

The first couple days after surgery, it is typical to feel pain. During surgery, medications such as steroids are infused into the area to help reduce swelling. The medication eventually wears off but your body continues to heal itself. During this initial healing phase, you will notice quite a bit of inflammation which may result in increased pain.
Usually, this is a temporary set back. As you heal, your body reduces the swelling and it should become less painful.
For discectomy surgery, the nerves may need to be moved away from the site of disc herniation. This can stretch the nerves and, for a small percentage of patients, this stretched nerve can cause numbness, pain, or even weakness of the muscles associated with that nerve. For the vast majority, this resolves over time.
During surgery, the manipulation of the nerve may have the unintended effect of further irritating it. This can cause the swelling to worsen and result in increased pinching of the nerve. So although the herniated disc or bone spur is removed, the nerve is still irritated. The nerve should eventually return to its normal size but if the pain persists, contact your surgeon to let them know.
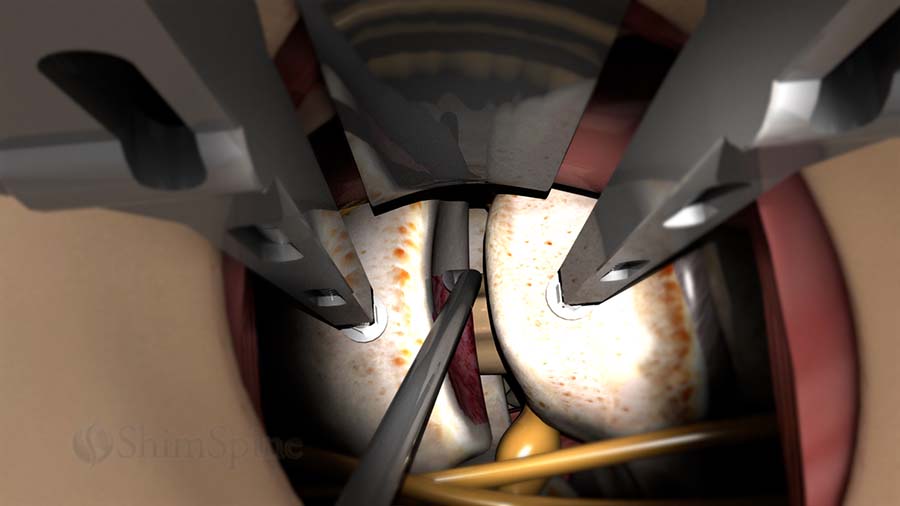
For fusion surgery, the bone edges need to be scraped to promote bleeding. The additional blood flow is necessary for the fused bones to heal. As explained in a previous blog, fusion is a process that results in the body treating two bones as one, similar to a broken bone. Understandably, this scraping can be a source of pain. However, as the fused bones mature, it should become less painful.
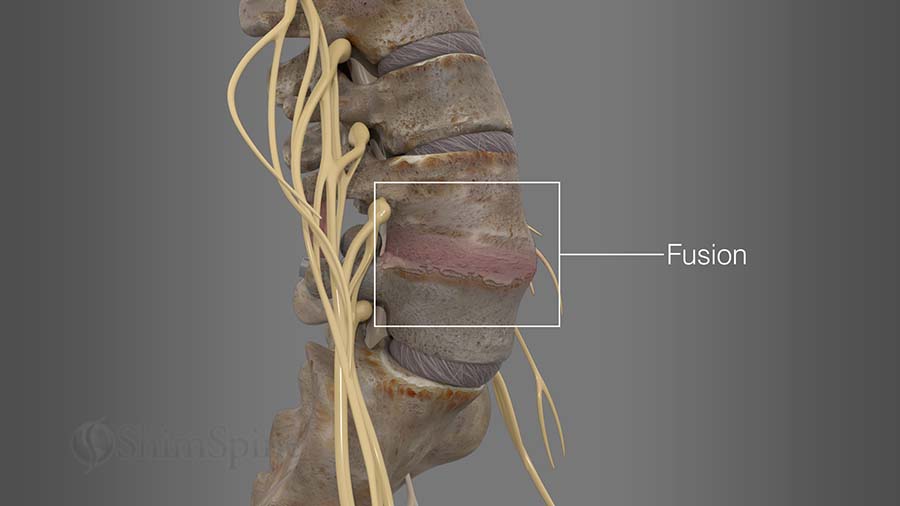
A combination of rods, plates, and screws are used to hold the bones in place while fusion takes place. Before it’s complete, the bones may still move around and continue to cause you pain. However, once fully fused, your condition should improve.
For some people, the immediate relief following spine surgery is short-lived. As your body heals, scar tissue will form on your nerves and this may cause you pain when you make certain movements. Further testing can reveal increased scarring of the nerves. The scaring tethers the nerves, causing pain with motion. If this is the case, every attempt should be made to stretch the scar with exercise — as this will allow more give to the tissues, and allow you to move without pulling on the nerves. Unfortunately, additional surgery to free the scarring will just result in more scarring.

For some people, the scarring associated with the incision, along with the atrophy of the muscles dissected during the operation can be a source of pain.
For all surgery patients, the pain from having surgery can take several weeks to resolve. Most of the time, any increased or lingering pain is temporary. Most of the time, the surgery itself is successful and you just need to give your body time to recover.
However, for some, the source of pain might warrant serious concern.
Next week’s blog will follow up on this topic and discuss the most common complications in spine surgery.
Citations
- Lebude B, Yadla S, Albert T, Anderson DG, Harrop JS, Hilibrand A, Maltenfort M, Sharan A, Vaccaro AR, Ratliff JK. Defining "complications" in spine surgery: neurosurgery and orthopedic spine surgeons' survey. J Spinal Disord Tech. 2010 Dec;23(8):493-500. PubMed PMID: 20124913
- Zeidman SM, Ducker TB, Raycroft J. Trends and complications in cervical spine surgery: 1989-1993. J Spinal Disord. 1997 Dec;10(6):523-6. PubMed PMID: 9438819
Last modified: October 15, 2020










Thanks Dr after endoscopic disk surgery at L4 L5 and S1 still there when walking. Can gym help recovery? It’s now it’s now 8 months after that surgery.
Had spinal senoies had operation 9 weeks ago pain has come back worse will I ever be better
I have done with L4L5 surgery and its almost 4months know.still i have sevirour pain.
I’m 3 weeks post op on a S1 disectomy/lamanectomy. My pain has steadily gotten worse over the last 4 days. I’m on 7.5mg oxycodone every 6 hrs with Cymbalta and still in extreme pain like before my surgery. My surgeon says it’s normal and the blood from the surgey is releasing into my internal incision area causing more inflammation probably. He said take 600mg ibprophen every 8 hrs. I started last night and took a 15mg oxy at 12am. I woke up in extreme pain around 5:30am. My buttocks/leg is on fire ? ? is this truly normal to be in this much pain JUST LIKE before surgery at week 3 and it getting worse everyday? Even when I up my medication intake so much?
I suffered severe dizziness and dysequilbrium for 4 years with extensive workup but no etiology was ever identified. My symptoms disappeared after surgery. Could you please address cervicogenic dizziness in one of your blogs? I wonder how common this is and suspect it is significantly under recognized. Could you please email me when it posts? Thank you!
I suffered severe rebound pain following a 2 level cervical fusion more that 3 weeks postop that was radicular and just as severe (9/10) as my preop pain, but on the opposite side as preop pain. It started suddenly during the night. I was told it was rebound pain during an uneventful postop recovery and that this was not unusual. Could you please write a blog about this and email me when it posts? Thank you!