Disc Herniations or Slipped Discs Get Better Without Surgery
Most disc herniations or slip discs get better without surgery. In fact, many herniated discs do not even cause pain. I know, not what you are told by others. But, it is the truth.
Many research studies show herniated discs are found in many people who have no pain associated with the finding.
But, if you do have herniated or slipped disc pain, know that most disc related pains improve and go away.
If we review how herniated discs happen, the most simple way is to use the jelly donut model.
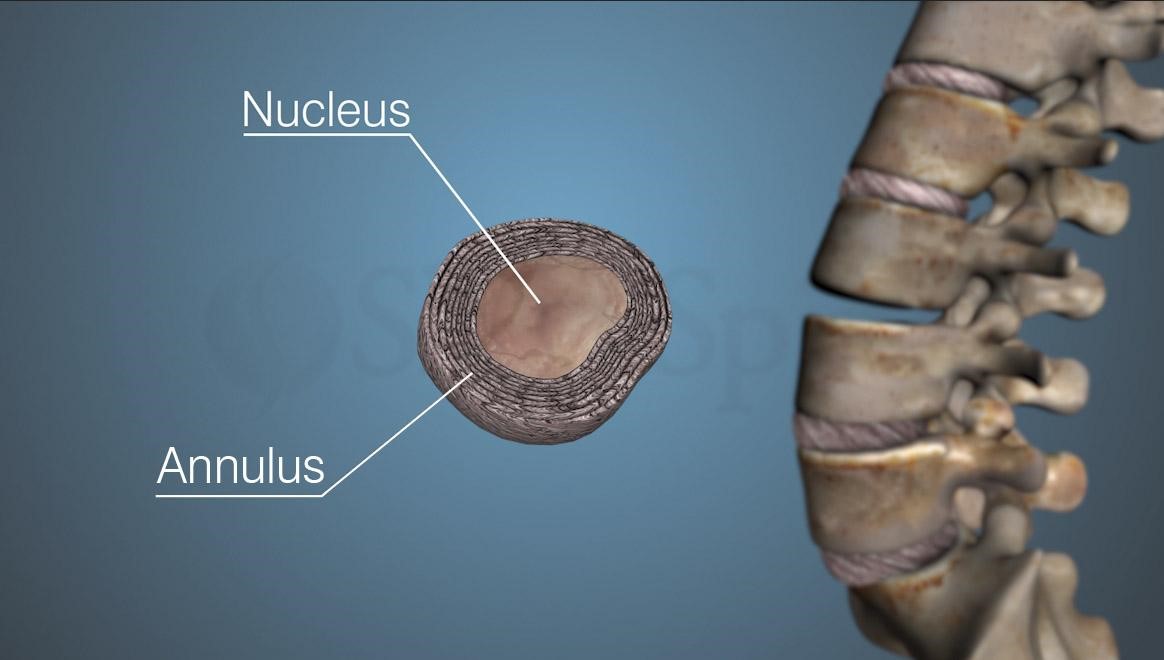
The center of the human disc, which is the nucleus pulposus, ruptures through the annulus fibrosus, which is the woven structure containing the nucleus. The nucleus, which has chemicals as well as a mass, irritates the surrounding tissues, including the nerves. It is like the jelly coming out of the side hole of the donut.
To be a bit more specific, the outside structure, the annulus fibrosus, is made of crosslinked woven fibers, that criss cross and and are tied to each other, thus holding in the center “jelly” or nucleus pulposus.
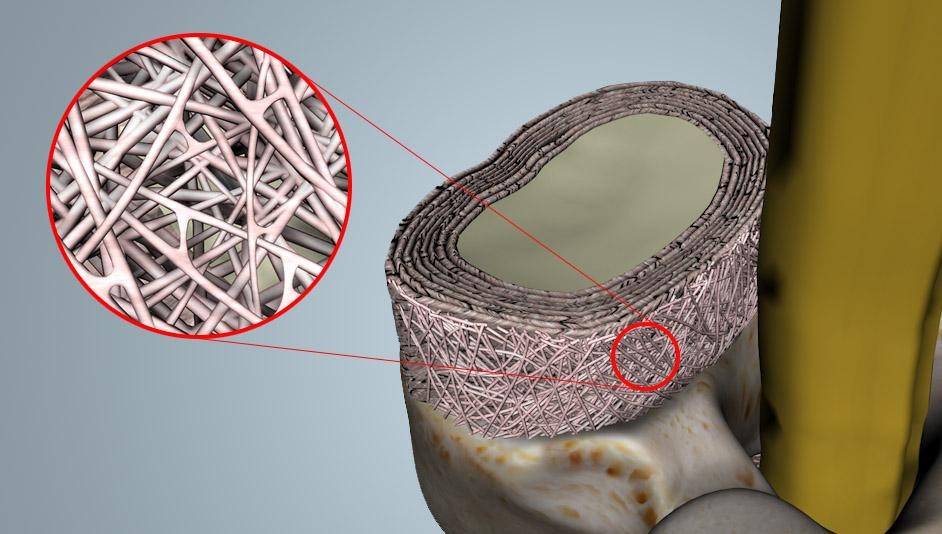
The crosslinks of the fibers may break, allowing a separation of the fibers, and the nucleus can push through that break. Once that weak spot allowing an opening, the fibers themselves can also break, causing a blow out of the nucleus. The nucleus material causes an inflammation of the tissues and nerves, and the mechanical pressure of the jelly like substance also compresses the nerves and tissues. That causes the pain signals, numbness, and weakness. Ouch!!
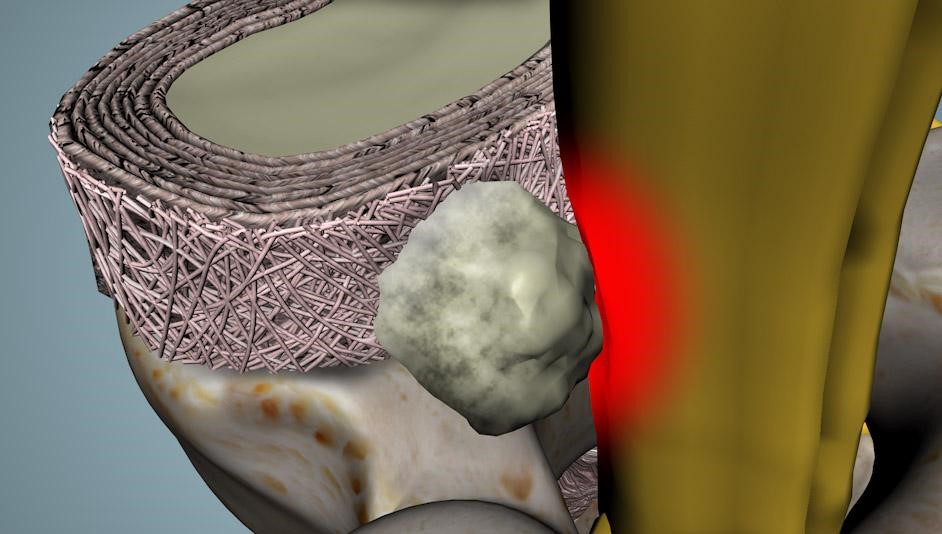
So, how does the body fight off the pain associated with the disc herniation?
The human body removes any foreign objects by activating special cells called macrophages and monocytes that attack and destroy foreign material. To use another analogy, these cells are like small Pac-Men, that chomp away at that stuff.
To the body, a herniated disk, which is the nucleus pulposus in the wrong location , is considered a foreign object. The macrophages and monocytes pacman away the nucleus. In addition, the largest disc herniations tend to have the most water content. With time, the disc piece will dehydrate. Over time, the disc herniation is removed, and shrinks back so it does not irritate the nerves or the tissues. The body also heals back the tear in the annulus, and re-ties the annular fibers. That healed annulus is now associated with a scar, and though it helps hold the nucleus back into its position, it is a weaker area, and has small but increased change of rerupture. The disc will continue with the natural dehydration process and will bulge over time. That is why if you get serial MRI studies of large disc herniations, you will see spontaneous regress of the herniation, and longer term, the findings of a disc bulge.
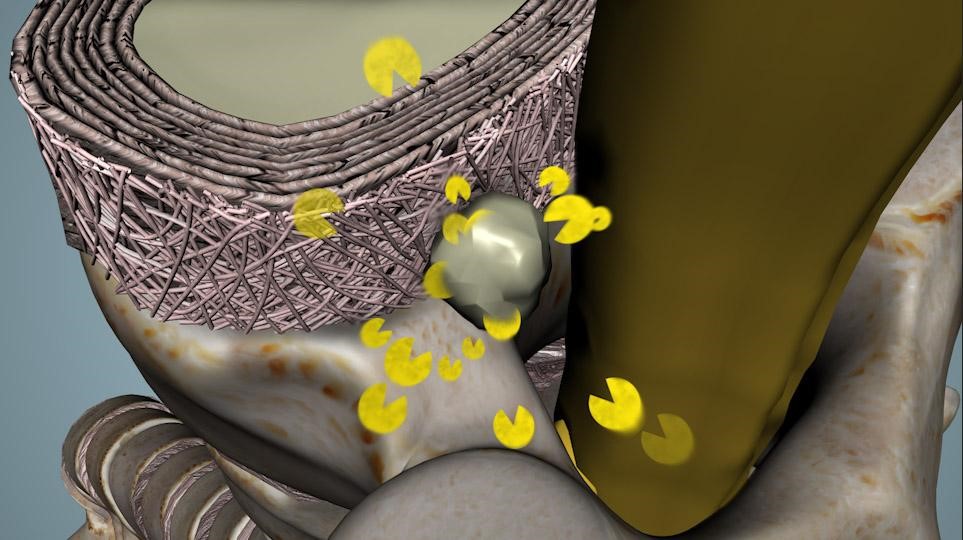
The most important thing you need to know is that the body does have it’s own way to remove disc herniations. If you are patient enough, and do not have major nerve issues that require surgery, most of the time, the body does remove the disc herniation on it’s own. This is the reason why many people will have disc herniations or bulges on MRI without any pain.
If you are in severe pain, please discuss your condition with a doctor to make sure you do not have a situation that requires urgent, or emergent care. Fortunately, these situations rarely occur. On the other hand, if you have true loss of muscle strength, loss of the ability to control your bowels or bladder, you may need care right now.
If your doctor determines that is not the case, if you can tolerate the current pain, allow your body to start the process of removing the disc herniation. Let your body Pac-man that disc.
If you are in pain, but do not have any significant loss of body functions, you can wait to see if your body will remove or improve the disc herniation. That is why greater than 90% of people with disc herniations do get better after 6-8 weeks. NO SURGERY needed.
Take HOME MESSAGE:
If you can tolerate the pain and be patient, you can avoid disc surgery.
Citations
- Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990 Mar;72(3):403-8. PubMed PMID: 2312537
- Demirel A, Yorubulut M, Ergun N. Regression of lumbar disc herniation by physiotherapy. Does non-surgical spinal decompression therapy make a difference? Double-blind randomized controlled trial. J Back Musculoskelet Rehabil. 2017 Sep 22;30(5):1015-1022. PubMed PMID: 28505956
- Yang X, Zhang Q, Hao X, Guo X, Wang L. Spontaneous regression of herniated lumbar discs: Report of one illustrative case and review of the literature. Clin Neurol Neurosurg. 2016 Apr;143:86-9. PubMed PMID: 26907997
- Chiu CC, Chuang TY, Chang KH, Wu CH, Lin PW, Hsu WY. The probability of spontaneous regression of lumbar herniated disc: a systematic review. Clin Rehabil. 2015 Feb;29(2):184-95. PubMed PMID: 25009200
- Macki M, Hernandez-Hermann M, Bydon M, Gokaslan A, McGovern K, Bydon A. Spontaneous regression of sequestrated lumbar disc herniations: Literature review. Clin Neurol Neurosurg. 2014 May;120:136-41. PubMed PMID: 24630494
Last modified: October 17, 2019










Hi Doctor Shim,
During the time of disc healing is it better to rest or mild exercise?
Hello Doctor,
I am a 22yr old student and preparing for defence forces job.
Last year in april i got this injury while doing deadlift and Squats just a day after deadlift,
later in MRI reports it showed “Breech in Pars Interarticularis of L5 seen with Grade I spondylolisthesis of L5 Over S1 With Diffuse Bulge of L5-S1 Disc With Thecal Sac Identation”
so i took rest with medicine for months and it went well but in some times or after some months pain comes again and again so is this normal and still self healable or i need some serious medical attention on this issue. because this particular video really gave me hope.
Waiting for your reply sir 🙂
Mr. Singh, thank you for your services to your Country and to the military. I have treated many soldiers and I have some concerns if your MRI shows a pars break, and a Grade 1 Spondylolisthesis. Many people have a spondylolisthesis and it can be found in up to 7% of the earths population, with no long term problems. But if the pars breech is recent, or more active, you should consider a formal evaluation by a spinal specialist. I am sure you will be fine, but an evaluation by a doctor is better than looking for advice on the internet. Good luck and much respect for your service.
My 32 yr old daughter has severe lower back pain that continues to get worse it is extreme difficult for her to go to work and sit at her desk all day, and now she can barely get dressed because the pain is so severe
She has gone to a orthopedic bone and joint center where she has been seen by several doctor’s who are treating her based on a scan from two years ago that showed a herniated disc she was sent her to physical therapy which seemed to make it worse if not worse it definitely did not make it any better and the physical therapist found it odd that it hadn’t helped her at all
my concern is if this scan is 2 years old then its possible that it may not be a herniated disc that’s causing her pain it could very possibly be something new going on , from what I’ve read on your website if I’m understanding correctly a lot of times herniated disc can heal themselves so its probably not a good idea to be treating her based on a scan that’s two years old and she probably should get a new MRI- do you think that this is something that should be brought to the doctor’s attention or is it possible that she can be treated based on the results of MRI that was done two years ago? I just think that there might be something else going on!
they are planning to give her steroid injections next since PT didn’t help.
My daughter is in so much pain that at this point she’ll try anything I’m afraid that this course of treatment may not be best for her I know you can’t give medical advice but any suggestions would be greatly appreciated
Shannon,
I am sure you are very concerned. MRI’s by themselves may not be as useful. A complete evaluation will give doctors information to determine the next steps in ordering tests. Please consider a second opinion with a doctor who knows nothing about her prior treatments. Then, when they take the time to obtain the history and perform a physical, they can view the information as a clean slate instead of relying on information that may no longer be relevant to your daughter’s condition. The doctor’s may then come to the same conclusions, but at least this time, you will know that the treatments were not based on a 2 year old MRI. I hope she gets better, and you have some peace of mind.
Thank you Dr. Shim for this valuable information. I was so happy to see your video. It made me feel a whole lot better.
I hope you will get better over time. There are always more aggressive options, but know that many disc herniations do improve with time.
Thanks for the post keep sharing.
I’ll ask a simple question first, then in a few days, ask a more detailed question. L5 nerve root… 5 weeks numbness on lateral, fibular surface, and numb sensation when standing on bottom of foot. If the numbness changes to a prickling sensation, is that getting better or worse? Generally is the change to prickling or sharp from numbness a sign of improvement or deterioration?
Excellent question and a common one from folks I treat. The answer is not an easy one. There are two general responses. 1. It is getting better as the nerve is less irritated therefore providing its normal response of heightened sensation. 2. there may be a change to the nerve by a change to the size and shape of the disc, or bone spur. Either way, the most significant concern would be progression of pain, development of weakness, or loss of ability to control your bowels or bladder (you soil yourself without control). If you are experiencing overall less pain, and have the ability to resume more “normal” activities, it is likely you are getting better. But I am speaking in generalities. To get answers about your individual situation, please talk to your doctors about YOUR conditions. Thanks for the comment and question.
Thanks for all these explanations .I’d like to know if I have done right or not . I had a loss of the strength of my heel and a kind of paralysis I couldn’t stand on my heel , so I made a surgery to free the nerve and fixed the lumbar with screws. Please just answer me if it was necessary to do so or just a big mistake. Thanks .
I hope you would have that discussion with your own doctor. Frankly, if you are improving, then you have your answer. I hope you continue to improve.
I like this,Tank you because I have a disc problem
Hi, I m suffering from this disc herniation n bulge since 4 moths. I m now able to walk but the pain is still in my right side effected leg from my hip to toe. I used medicine n exercises adviced by doctors but the pain is still on. More 6 weeks wait they said to me. My neurologist said that there is no major issue in my MRI. So plz tell me what should I do? Thanks
Unfortunately, I cannot give anyone specific advice as each situation is individual. In general, most disc herniation symptoms do improve over time without the need for surgery. If the situation becomes intolerable, then seen the attention of a surgeon and discuss your options. Be advised, however, that surgery can never be guaranteed. I have performed thousands of spinal surgeries and procedures. I wish I could tell you that 100% got better, but that could never be true. Remember that there are risks. Impatience causes many to pursue riskier options.
Thank you for producing this video. I have a herniated disk (L5, S1) and after six months of daily exercises, chiropractic, acupuncture, physical therapy, and an epidural injection, I’m no better.
I’m 64. I understand that surgery is an option but want to avoid it for all of the reasons I’ve read about. Can I or will I heal as you mentioned in your video? You said 90% will heal. Is there a (small) percentage that has no option and must get surgery for relief?
There are certain circumstances where you must get surgery to avoid permanent loss of important body functions. In that circumstance, at least in the USA, a surgeon will firmly state you should get surgery, and if you do not, the Surgeon will discharge you from care as you are making a serious decision against medical advice. You will need to sign a document to say so, and that you will take responsibility of the consequences. Fortunately this is a very rare situation, and usually involves infections, tumors, and unstable fracture configurations that could lead to a permanent paralysis condition. In rare circumstances, it is because of a disc herniation that is causing bowel/bladder dysfunction, or inability to control the muscles to the legs. In most circumstances, it is a gradual, chronic condition that can be painful, annoying and preventing you to do important things in your life. If it becomes a big enough issue, then most will explore their options including surgery. Unfortunately, there can never be any guarantee that the surgery or any treatment will help. Do the least risky first. Many times, the pain lessens and you do not need to do anything more. If the situation is progressive, then surgery sometimes can be an option. But please get proper counseling from a Doctor you trust.
Hello DR Shim,
Have a slip disc herniated disc with extrusion but with mild pain I can walk stand but not sitting a lot is this will heal with a time ? Regards
Sounds like you are already healing.
Hello, Dr,
I believe there exists in our body a self-repairing mechanism that can heal our herniated disc.
This is because I have had such an experience. But, it took me more than two years to get my herniated disc healed by my body.
The following is what I have experienced :
In July 1997, I had nerve pain starting from my buttock and travelling down to my leg. I went to see a doctor who told me I had disc protrusion on L4/5. From then on, I had to undergo a long period of struggling with the nerve pain.
In 7/1998 (one year later), I saw another doctor who asked me to conduct an MRI scan. Surprisingly, no disc protrusion was found. I was very happy to hear that “normal” result. However, after one month (in 8/1998), I began to have the nerve pain that I had had before. I then went back to ask the doctor why. This time, he told me that there were some cracks in my disc but they were too small to be detected by the MRI scan. I was so unhappy to hear that.
After that, I had to live with the pain. In 9/1999, another doctor suggested me to conduct an MRI scan. This time, the scan showed I had my disc protruded on L4 & L5.
However, to my very great surprise, the nerve pain associated with the disc herniation was gradually declining. I remember I could sit for long hours without any pain after about four to five months. I could lead a normal life for about 21 years.
Unfortunately, in 12/2020, I found I had the same nerve pain again. I went to see my doctor who told me my disc protruded again. I am now suffering from the pain.
I am a male aged 56. Twenty one years ago, I was aged 35. I am now order than before by slightly more than 20 years. Naturally, my metabolism now is slower than that of being a 35-year-old man.
I want to ask the questions that, I think, are very important for me :
Does a person like me who has got his/her herniated disc healed by his/her body still have another chance to get this self healing mechanism ?
In other words, will I still have a second chance to get my herniated disc healed by my body ?
Suppose the answer to the above question is yes. But, I am in my mid-fifties, having my metabolism more sluggish than before.
Does this affect the self healing mechanism ?
Thanks
I am looking forward to receiving your reply.
Yes.
I have been diagnosed with a very subtle anterior osteophytes Seen on L2-L5
I am having a sever pain in my lower back, am 53yrs old
Pls how can you help, I live in Nigeria West Africa
Regards
Please get you condition evaluated by a doctor you trust. Subtle osteophytes, by themselves, are usually not the source of such pain. It may warrant further investigation.
Good day Dr. Iive in Nigeria, I was to assist in lifting a small refrigerator on 17th December 2020, i feel a very sharp pain in my back and temporary seizure of my left leg before I could move, i have x-ray on Friday 18th December 2020.
Radiology report reads.
LUMBOSACRAL SPINE(AP+LAT)
THERE’S LEFT SIDED LUMBER SCOLIOSIS
THERE IS LOSS OF NORMAL LUMBER LORDOSIS WITH MARGINAL BONY OUTGROWTHS (OSTEOPHYTES) ON L2-4 WITH ENDPLATE SCLEROSIS.
THERE IS SCLEROTIC NARROWING OF L5S1 DISC SPACE.
THE POSTERIOR ELEMENTS APPEAR NORMAL.
CONCLUSION :TRAUMATIC SPONDYLOSIS
I can only give general comments, and without looking at the images, I can only comment on the reading. It basically says that you have developed arthritis of the back. Spondylosis means arthritis changes. I am not sure how the word traumatic relates to your reading as there is no comment on evidence of any prior broken bones in the spine. This is a very common report, and does not give any indication of why you have a left leg pain, other than it shows osteophytes, which are slowing growing bone spurs that takes months if not years to develop. It is possible the bone spurs are causing some nerve irritation, but is may not have anything to do with your current complaints. Please followup with your doctor to discuss.
I have had my pain, numbness, tingling my left leg/lower back sometimes feet pain, burning sensation for almost a year now on and off with pain meds and muscle relaxers. Probably re-injured myself during this timeframe and gotten worse. However, I just recently had my MRI done and was shown to have Mild degenerative disc disease (minimal disc bulge) at L5-S1 with small annular fissure in the periphery of the disc to the left midline. Knowing that I probably re-injured my back, how long would it take for my tear and disc bulge to heal? I’ve done a few stretching exercises here and there, and seems to make the problem worse.
Sorry to hear you are not doing as well as you would like. I can only give general information and not specific advice to you. Many people will have findings on MRI’s, but not all the findings are the cause of pain. That is a very common issue with spine MRI’s. The normal process of aging will include disc degeneration, and narrowing. That narrowing process is how people become shorter as they age. Exercise, and stretching is always helpful, but can transiently increase the pain. If you have nerve irritation pains, see your doctor about advice. If you do not, sometimes it will take some time ( several months), but eventually, more than 95% of people do get better after a herniated disc. If you are in the 5%, please get it evaluated.
Sir, i do have the similar condition. It’s been 6 weeks from this getting bad and i started to have bed rest. But even now can i feel the pain if i do something by bending. Will it get cured by a few more weeks!!?
In general, most people do get better with time. But, if you are getting worse, please get it evaluated by a doctor.
Dear Sir, I have diffuse bulge of C 3-4, C 4-5, C 5-6 and C 6-7 discs indenting the anterior thecal sac.
Diffuse bulge of D 4-5, D 5-6 indenting the anterior thecal sac.
Ligamentum flavum hypertrophy noted at D 9- 10 and D 10- 11 levels, indenting the posterior thecal sac.
Diffuse bulge of L 4-5 disc, indenting the thecal sac, bilateral exiting nerve roots with narrowing of bilateral neural foramina.
Diffuse bulge of L 2-3 and L 3-4 discs, indenting the thecal sac.
Sir, please suggest me the exercises I have to do. Thank you Sir.
https://youtu.be/IKVlz07Eqis
I have herniated disc L5 S1 no more pain in my right legs and my MRI shows I have no nerve or rute issue it’s already 6 month since the accident now only minor pain daily in my lower back shifting to my SI Hip Joint. How many more months do u think I will fully recover as long back to the sorce my disc
It’s a two steps forward and one step back kind of thing. You feel good, you do something that causes a little swelling, you hurt again. There is no timeline on this, but it sounds like you are actually improving. Ice after activities, and knowing to avoid what sets things off, will speed up your recovery.
Hello Dr.,
I have had a fall during soccer back in 2003. Ever since I have had perennial sharp severe pains in my waist. There is nothing to show in a scan but the pain returns each year and goes away in a week. Could you advise me on how to stop this permanently? could it be a disc herniation or tear?
I’m sorry. We cannot give personalized medical advice without actually seeing a patient. A diary of what you do physically before this pain starts would help your treating physician with a diagnosis.
I have problem with my right leg , I feel my right leg no strong like my left leg , and I feel some pain in my right leg , and when I am going it is some of the pain also when I am setting
This pain and weakness could be originating in your back, Masood.It would certainly be a good idea to have it examined.
Hello doc this was such an encouraging video.
I am currently having stiff back with pain radiating towards my right leg. Do i need to wait for 6 to 8 weeks and let the body function?
I am taking muscle relaxant and pregabalin at the moment along with Vitamin D and Cac.
As long as you are not having neurological deficits, time is your friend. Gentle stretching and strengthening can help.
I have a bulge L5/S1 left side with pressure on the nerve root (MRI) but no intense pain. However, when I try to walk my glutes and lower back tighten and spasm. This has been the case for 2-3 months. It is slowly improving with some good days and some days back to normal. Could it be a Piriformis issue vs nerve?
We could not diagnose this without actually seeing you. As you are improving, keep up with mild exercise and ice afterwards. It usually takes at least 3 months for things to settle down.
Sir, is there any exercise need for disc bulging on L4,L5 if so please suggest.
Thanks
Please review the exercises on the front page of our website, shimspine.com
Dr. Shim I have herniated disc in my lower back what foods, would produce more macrophages and monocytes. Should I be on low calorie diet and would 16 hour fast help? I love your video’s there very clear.
Our biggest advice is to watch your weight and go low calorie if you need to lose a few pounds. Consulting a dietician for information would assist you.
my wife is suffering spine problem. She had surgery in 2006. Due to pain she can’t walk. Both legs and nerve not working. any solutions for Her. –Mathuradas Bhinde
We are unable to advise or treat patients we have not seen in person.
I have herniated disc L5_s1
Low back pain and buttock ,muscles spasm or thigh and leg ,pain is tolerated without pain killers for 6 months now .. will it heal or not ?
We usually give it 3-6 moths to heal. You may have some residual pain you will have to deal with, either medically or surgically.
Is there a way to improve or enhance the natural process of clearing disc bulging?
If we only knew Jamal! The biggest thing we recommend is to avoid hurting yourself again and strengthen your back with exercise.
I’m having back pain and numbness in my back foot and lap that makes it hard for me to walk a long distance. Please help
We are unable to advise or treat patients we have not seen in person. Please see your physician.
I have l4 l5 disc prolapse and numbness over my feet and mild weakness over my right lower limb.what is the physiotherapy ?
We would not presume to tell you the appropriate exercises. Please consult a trained and licensed Physical therapist for that information.
I have a bulging disc in L4L5. I feel pain on my lower back, buttock hips also on my knees. How can i do for all of this pain? Is basketball prohibited for bulging disc?
Basketball is not advised for anyone having back pain. Less “pounding” type activity such as walking or swimming is a much better idea.
I’m experiencing hot feet or burning feet, because of nerve damage and bulge in a few discs, how do I go about this problem.
bilateral foot burning would not be a normal response to a “bulging disc”. There are many other causes of this including diabetes, circulatory problems or side effects of medication. Please see your medical provider for diagnosis.