Herniated Disk | Sciatica (Slipped Disk)
Herniated Nucleus Pulposus
(Herniated Disk or Slipped Disk)
Typical patient presentation includes onset of back pain with leg radiations. This is the typical presentation of SCIATICA (slipped disk). A history of significant trauma is not necessary. Human physiology studies indicates the forces placed on the lumbar disc, is very significant for even trivial events. Activities of daily living, including sitting, bending over to pick up a newspaper, light lifting, and sneezing are associated with large intradiscal pressures that can lead to disk herniations (slipped disk).
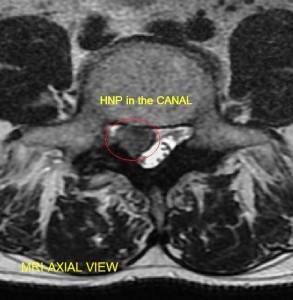
Patients complain of back pain, difficulty sitting, and radiating pain and numbness to the legs and feet. In slipped disk that project onto the thecal sac (nerve sac) , or exiting nerve roots, there may be a “pinched nerve” sensation. That includes numbness, reflex changes, and at times, muscle weakness. In rare but significant instances, the cauda equina of the spinal canal can be entrapped, causing impairment of bowel and bladder function. In simple terms, you loose the ability to control your urination and bowel movements. You soil yourself. In this scenario, patients should present urgently for medical help, and diagnostic workup. Call your doctor immediately, or go to the emergency room. The so-called cauda equina syndrome can be a permanent loss of bowel or bladder function if not properly managed. Often times, it requires surgical decompression of the nerves.
For patient without cauda equina syndrome, or progressive weakness, the treatment of choice remains nonsurgical care. Treatment options include judicious use of narcotic medications, oral steroids, nonsteroidal anti-inflammatory agents, physical therapy, chiropractic care, and epidural steroid injections. There are complimentary medicine options that may also be beneficial.
In patients that do not have cauda equina syndrome, or progressive weakness, or history of significant trauma, neoplasm, or infection, extensive diagnostic workup is not necessary for the initial 6 weeks. There are multitudes of studies indicating that the use of diagnostic x-rays are not necessary for initial management of a slipped disk. MRI scanning should be reserved for patient’s who do not improve with at least 6 weeks of noninvasive treatments.
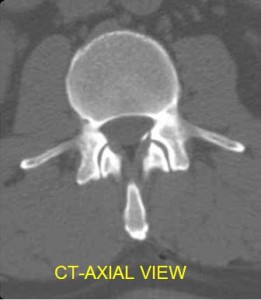
CT scans are helpful to define fractures of the spine. In a nontraumatic situation, it is not the first choice of diagnostic testing for disc herniations, unless there is a medical contraindication to the use of the MRI.
For the past few years, many insurance carriers no longer process requests for MRI or CT from primary care physicians. Often times, a referral is made to a spinal specialist. Based on the specialist recommendation, further diagnostic testing may be authorized to better define the slipped disk.
Last modified: October 22, 2019